"The fight against sickle cell is a fight for humanity."
Obi Light Ogbonnia
Sickle cell disease (SCD) is a group of inherited blood disorders that profoundly alter the shape and function of red blood cells. Affecting millions globally, this condition is a stark example of how genetic mutations can disrupt lives while also driving groundbreaking medical advancements. Here’s a closer look at its causes, challenges, and the evolving landscape of treatment.
What Causes Sickle Cell Disease?
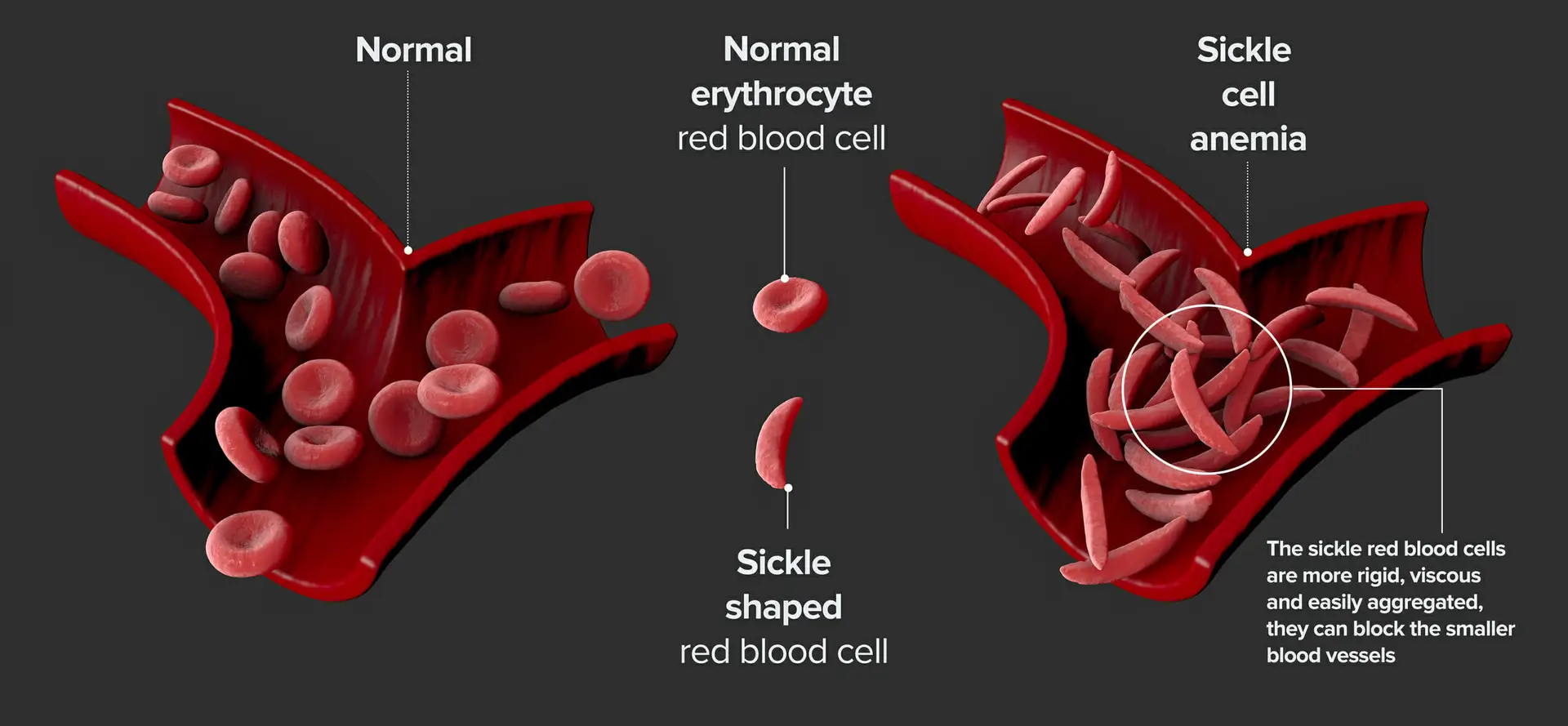
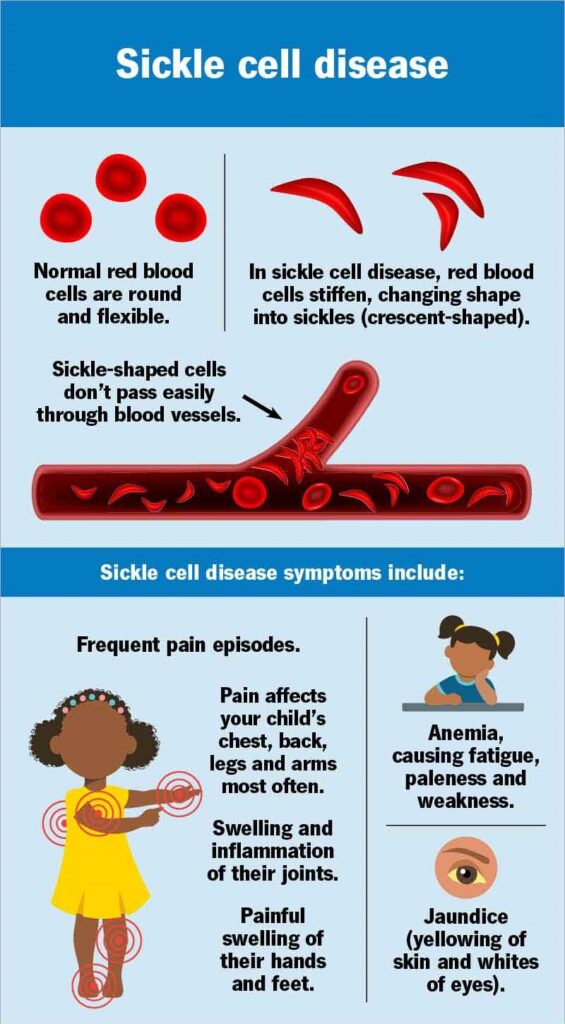
SCD stems from a genetic mutation in the HBB gene, which produces haemoglobin—the oxygen-carrying protein in red blood cells. This mutation causes haemoglobin to form rigid, crescent-shaped cells that obstruct blood flow, leading to tissue damage, pain, and severe complications. For a child to inherit SCD, both parents must pass on a defective gene. Those inheriting one gene have the sickle cell trait, typically asymptomatic, but capable of passing the gene to offspring
Symptoms and Complications
SCD manifests early, often by months of age, with symptoms varying in severity:
Pain Crises: Sudden, excruciating episodes caused by blocked blood flow, requiring emergency care.
Anaemia: Fatigue, jaundice, and paleness due to rapid red blood cell destruction.
Infections: Damaged spleen function heightens vulnerability to pneumonia and other infections.
Organ Damage: Blockages can lead to stroke, acute chest syndrome (lung failure), and vision loss.
Without treatment, life expectancy is reduced, though advances in care now enable many to live into their 50s or beyond.
Diagnosis and Prevention
Newborn screening programs, widespread in the U.S. and U.K., allow early detection via blood tests. Prenatal testing, such as amniocentesis, identifies SCD during pregnancy. Genetic counselling helps carriers understand risks and reproductive choices, aiming to reduce transmission.
Treatment Breakthroughs
While there’s no universal cure, therapies focus on symptom management and complication prevention:
Medications: Hydroxyurea reduces pain crises by boosting fetal haemoglobin production. Newer drugs like voxelotor prevent sickling, and crizanlizumab improves blood flow.
Blood Transfusions: Used to treat severe anemia or prevent strokes.
Gene Therapy: In 2023, the FDA approved CRISPR-based therapy (Casgevy) and Lyfgenia, which modify stem cells to produce healthy haemoglobin.
Bone Marrow Transplants: Potentially curative but limited by donor availability and risks
A Global Health Challenge
SCD disproportionately affects people of African, Mediterranean, and Middle Eastern descent. In the U.S., 1 in 365 Black newborns has SCD, compared to 1 in 16,300 Hispanic Americans. Globally, over 8 million are affected, with Nigeria alone accounting for 150,000 annual births.
Poverty, limited healthcare access, and stigma exacerbate suffering, highlighting the need for equitable care and education.
Hope on the Horizon

Advances in gene editing and personalised medicine offer unprecedented optimism. Researchers aim to expand CRISPR-based therapies and improve affordability.
Meanwhile, advocacy groups like the Obi Ogbonnia Sickle Cell Foundation tirelessly work to support patients and families
In Conclusion
Sickle cell disease is more than a medical condition—it’s a call to action. Through awareness, research, and global collaboration, we can transform survival into thriving. As Obi Ogbonnia, a 51-year-old SCD warrior, reminds us: “Alone, I survived. Together, we can ensure others thrive.”
References:
National Heart, Lung, and Blood Institute: Sickle Cell Disease: What Is Sickle Cell Disease?|September 30, 2024
CDC: About Sickle Cell Disease|February 21, 2025
NHS: Sickle cell disease|November 30, 2022
Britannica: sickle cell anaemia|April 15, 2025
Cleveland Clinic: Sickle cell disease|August 3, 2023
American Society of Haematology: Sickle Cell Disease|July 12, 2024
Mayoclinic: Sickle cell anemia|December. 22, 2023